Contents
What Is Fungal Acne? – Causes & Treatments
Fungal acne, also known as pityrosporum folliculitis or malassezia folliculitis, is caused by an overgrowth of yeast within the hair follicles. This leads to breakouts, itching, and irritation on the affected areas. The condition can be quite distressing due to its discomfort and cosmetic concerns.
What is fungal acne?
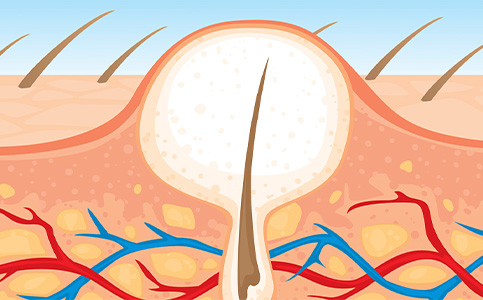
Fungal acne is an overgrowth of yeast within the hair follicles. Sebaceous glands within your skin produce an oil called “sebum.” These glands can overproduce oil, and your pores and hair follicle can become clogged with oil as well as bacteria and yeast that are naturally found on your skin. Bacteria can lead to the traditional acne blemishes, but the yeast causing inflammation of the hair follicles, or “folliculitis.” It’s not contagious, infectious or an indicator of poor skin hygiene.
What causes fungal acne?
Fungal acne is a bit of a misnomer. Unlike typical acne, fungal acne isn’t caused primarily by oil and bacteria in pores, although oil and sebum production are a big part of helping feed the bacteria that cause fungi.
Instead, the pimple-like bumps and irritated skin associated with fungal acne are caused by yeast overgrowth, a type of pityrosporum folliculitis. Yeast grow in warm, moist environments.
An imbalance or overgrowth of fungus levels on the skin can occur a variety of reasons including, but not limited to:

• Sweat
Wearing sweaty workout clothes for too long can trapped moisture and encourage yeast growth. Rewearing workout clothes without washing them may also expose your skin to fungi that have grown in the clothes.
• Hot and Humid Environment
Warm and moist environments. People living in hot climates, where sweating is more likely, may experience fungi acne more frequently.
• Use of Antibiotics and Steroids
Long-term use of topical or oral antibiotic such as clindamycin, doxycycline and minocycline will reduce the bacteria on your skin. Antibiotics cannot differentiate good or bad bacteria, so it kills all of it. That can allow for the overgrowth of pityrosporum folliculitis.
• Skincare Products
Yeast feeds on oil. If you are using skincare or makeup that contain certain types of fatty acid, oils, esters and some polysorbates, it could be a trigger even small amounts.
• Diet
While diet usually is not the initial cause of acne outbreak, once there is an existing imbalance your diet can play significant role, especially if it is high in sugar, fungi like yeast thrive on sugary carbohydrates. So balance your diet with fruits, vegetables and proteins to help discourage overgrowth.
Fungal Acne Symptoms
The most common fungal acne symptoms that you will notice is itchiness of the red bumps. This kind of acne is itchy but never painful, as typical acne can be when a blemish becomes inflamed. Fungal acne can be persistent, worsen with sweating, and flare in hot and humid temperatures. They often appears in small uniform red bumps in clusters on the upper chest, arms, back, and legs.
Your dermatologist will be able to diagnose this skin condition by its appearance, clinical symptoms and the lack of improvement with traditional acne medications. Skin scraping for yeast can be performed to confirm the diagnosis, if needed.

Treatment For Fungal Acne
Depending on the severity of the affected area, you may be able to clear up your skin by adjusting certain lifestyle habits. Showering immediately and changing into clean clothes after working out or wearing loose clothing can reduce acne like breakouts.
In severe cases, or if symptoms persist longer than three weeks, it may be time to schedule an appointment with your board certified dermatologist. A quick exam and skin scraping can tell your dermatologist all they need to know to offer you the right acne treatments option. Oral antifungal medication and topical acne treatment may be prescribed as they can target deep into the hair follicle. Side effects of medication and topical acne treatment are mainly minor from peer reviewed studies.
Oral treatment
Oral treatment is often the most effective option for treating fungal acne, especially when it comes to controlling the initial symptoms. Depending on the severity, your skin doctor will prescribe the most appropriate medication based on your current condition. The most common oral antifungal medication is Sporanox, whereas Accutane is often considered for more difficult cases.
Over-the-counter medication
While oral treatments are more effective, topical fungal acne treatments can be helpful for the maintenance and even prevention of future episodes of fungal folliculitis. Topical treatments often come in the form of an anti-dandruff shampoo that is to be used every day of the week or as per your doctor’s prescription. The most common treatments are Nizoral or Selsun, these are available in drugstores and online. They can be applied in the shower and left on for 5-10 minutes before rinsing off.
Prevention
While fungi acne cannot be prevented completely, these steps may help reduce the chances of a return infection:

Shower whenever you sweat excessively.
Change out of sweaty clothes right away.
Wear loose clothing.
Choose breathable fabrics.
Choose oil free moisturizer.
Balanced diet.
Use antifungal shampoo and body wash to remove dead skin cells.
Avoid unnecessary antibiotic, whether topical or pills. It is the best to talk to your board certified dermatologist so that they can advise the best treatment as well as effective treatment for you.
When to see a dermatologist?
If you have yeast infection, changing some habits and trying the over-the-counter acne treatments above may help to treat fungal acne. However, if your acne lasts longer than a few weeks, is getting worse or not improving, or makes you feel shy and embarrassed, you should see your board certified skin doctor. The skin doctor will work with you to develop a treatment plan that is right for you.

Conclusion
Fungal acne is a common infection and is usually easy to treat as long as it is correctly diagnosed. While managing fungal acne can be vastly different from managing the vulgaris acne that you are used to, fungal folliculitis can often be prevented with consistent personal care and hygiene to prevent yeast infection.
It is important to note that fungal folliculitis will not respond to vulgaris acne medication, and the use of these drugs may make it worse. If you suspect you have this acne infection, talk with your dermatologist or primary healthcare provider about what to do.




